Revisión: Infección natural por SARS-CoV-2 en animales
Palabras clave:
SARS-CoV-2, COVID-19, zoonosis, infección animalResumen
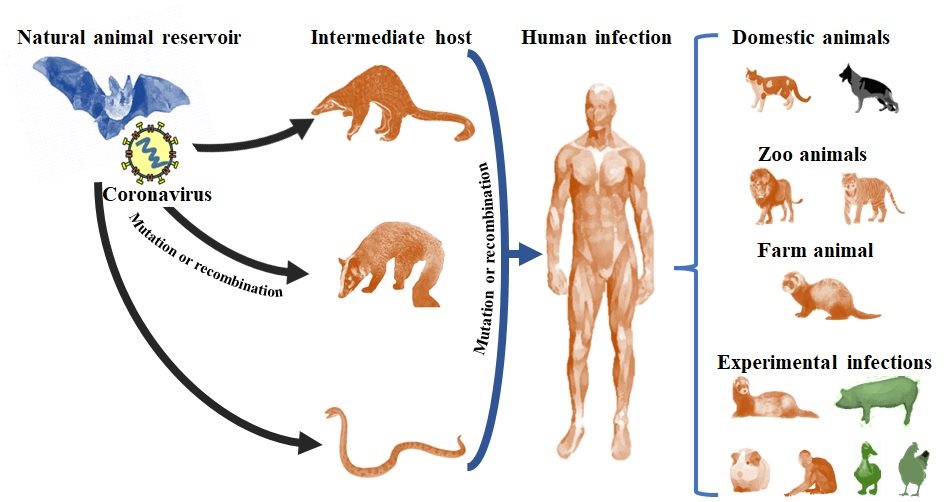
El objetivo de este estudio fue evaluar los informes epidemiológicos y patológicos de brotes y casos confirmados de la enfermedad por SARS-CoV-2 en animales de zoológico, granja y mascota infectados naturalmente. Se obtuvieron informes de brotes y casos de animales infectados por SARS-CoV-2 mediante búsqueda, análisis y clasificación sistemática de información disponible en bases de datos de libre acceso. Los informes se evaluaron e incorporaron a una base de datos, se clasificaron e integraron para identificar los valores característicos de morbilidad, mortalidad y manifestaciones clínicas del SARS-CoV-2 en animales; además de lesiones post mortem y alteraciones microscópicas. Se indican alternativas diagnósticas y terapéuticas para confirmar o mitigar la infección en animales; métodos de control como el aislamiento, sacrificio de poblaciones afectadas y las primeras vacunas disponibles para animales. La información disponible sugiere que los animales se han convertido en huéspedes accidentales del SARS-CoV-2, infectándose principalmente a través del contacto con personas afectadas por COVID-19; aunque existe la preocupación de que los animales podrían convertirse en un riesgo de mantenimiento y propagación de nuevas variantes virales, que eventualmente podrían volver a las poblaciones humanas.
http://dx.doi.org/10.21929/abavet2023.14
e2022-52
https://www.youtube.com/watch?v=pZyEFBQfKIo
Citas
ABDEL-MONEIM AS, Abdelwhab EM. 2020. Evidence for SARS-CoV-2 infection of animal hosts. Pathogens. 9(7):529. https://doi.org/10.3390/pathogens9070529
AHN DG, Shin HJ, Kim MH, Lee S, Kim HS, Myoung J, Kim BT, Kim SJ. 2020. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). https://doi.org/10.4014/jmb.2003.03011
ANAND KB, Karade S, Sen S, Gupta RM. 2020. SARS-CoV-2: Camazotz’s Curse. Medical Journal, Armed Forces India. 76(2):136.
https://doi.org/10.1016/j.mjafi.2020.04.008
BOUDEWIJNS R, Thibaut HJ, Kaptein SJF, Li R, Vergote V, Seldeslachts L, de Keyzer C, Bervoets L, Sharma S, van Weyenbergh J. 2020. STAT2 signaling as double-edged sword restricting viral dissemination but driving severe pneumonia in SARS-CoV-2 infected hamsters. BioRxiv. https://doi.org/10.1101/2020.04.23.056838
BULUT C, Kato Y. 2020. Epidemiology of COVID-19. Turkish Journal of Medical Sciences. 50(SI-1):563–570. https://doi.org/10.3906/sag-2004-172
CHAN JFW, Zhang AJ, Yuan S, Poon VKM, Chan CCS, Lee ACY, Chan W, Fan Z, Tsoi HW, Wen L. 2020. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in a golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clinical Infectious Diseases. 71(9):2428–2446. https://doi.org/10.1093/cid/ciaa325
CHAVDA VP, Feehan J, Apostolopoulos V. 2021. A Veterinary Vaccine for SARS-CoV-2: The First COVID-19 Vaccine for Animals. Vaccines. 9(6):631.
https://doi.org/10.3390/vaccines9060631
CHEN Z, Boon SS, Wang MH, Chan RWY, Chan PKS. 2021. Genomic and evolutionary comparison between SARS-CoV-2 and other human coronaviruses. Journal of Virological Methods. 289:114032. https://doi.org/10.1016/j.jviromet.2020.114032
CHOWDHURY SD, Oommen AM. 2020. Epidemiology of COVID-19. Journal of Digestive Endoscopy. 11(1):3. https://doi.org/10.1055/s-0040-1712187
CIOTTI M, Angeletti S, Minieri M, Giovannetti M, Benvenuto D, Pascarella S, Sagnelli C, Bianchi M, Bernardini S, Ciccozzi M. 2020. COVID-19 Outbreak: An Overview. Chemotherapy. 64(5-6): 215-223. https://doi.org/10.1159/000507423
DAS A, Roy S, Swarnakar S, Chatterjee N. 2021. Understanding the immunological aspects of SARS-CoV-2 causing COVID-19 pandemic: A therapeutic approach. Clinical Immunology. 108804. https://doi.org/10.1016/j.clim.2021.108804
D’CRUZ RJ, Currier AW, Sampson VB. 2020. Laboratory testing methods for novel severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Frontiers in Cell and Developmental Biology. 8:468. https://doi.org/10.3389/fcell.2020.00468
DE ANDRADE JF, de Lima Cruz IR, de Sampaio FMS, da Silva CGL, Lopes MR, Gadelha MSV. 2021. Pesquisa de SARS-COV-2 em cães e gatos: relatos de casos na literatura. Brazilian Journal of Development: 7(5):45198–45209. https://doi.org/10.34117/bjdv7n5-101
EVVIVAX. 2021. December 30). Evvivax and Applied DNA Veterinary COVID-19 Vaccine Candidate Induces Neutralizing Antibodies in 100% of Trial Cohort Against B.1.1.7, P1, and B.1.526 Variants. Https://www.Evvivax.Com/News.Html
FASINA FO. 2020. Novel coronavirus (2019-nCoV) update: What we know and what is unknown. Asian Pacific Journal of Tropical Medicine. 13(3):97.
https://doi.org/10.4103/1995-7645.277795
GAO J, Quan L. 2020. Current Status of Diagnostic Testing for SARS-CoV-2 Infection and Future Developments: A Review. Medical Science Monitor. International Medical Journal of Experimental and Clinical Research. 26:e928552-1.
https://doi.org/10.12659/MSM.928552
GUO YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, Yan Y. 2020. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Military Medical Research. 7(1):1–10.
https://doi.org/10.1186/s40779-020-00240-0
HALE VL, Dennis PM, McBride DS, Nolting JM, Madden C, Huey D, Ehrlich M, Grieser J, Winston J, Lombardi D. 2022. SARS-CoV-2 infection in free-ranging white-tailed deer. Nature. 602(7897):481–486. https://doi.org/10.1038/s41586-021-04353-x
HU B, Guo H, Zhou P, Shi ZL. 2021. Characteristics of SARS-CoV-2 and COVID-19. Nature Reviews Microbiology. 19(3):141–154. https://doi.org/10.1038/s41579-020-00459-7
ICTV (International Committee on Taxonomy of Viruses). 2021. https://talk.ictvonline.org/
IZDA V, Jeffries MA, Sawalha AH. 2020. COVID-19: A review of therapeutic strategies and vaccine candidates. Clinical Immunology. 222:108634.
https://doi.org/10.1016/j.clim.2020.108634
JALAVA K. 2020. First respiratory transmitted food borne outbreak?. International Journal of Hygiene and Environmental Health. 226:113490.
https://doi.org/10.1016/j.ijheh.2020.113490
JARROM D, Elston L, Washington J, Prettyjohns M, Cann K, Myles S, Groves P. 2020. Effectiveness of tests to detect the presence of SARS-CoV-2 virus, and antibodies to SARS-CoV-2, to inform COVID-19 diagnosis: a rapid systematic review. BMJ Evidence-Based Medicine. 27(1):33-45. https://doi.org/10.1136/bmjebm-2020-111511
JI W, Li X. 2020. Response to “Comments on" Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross‐species transmission from snake to human” and “Codon bias analysis alone is uninformative for identifying host (s) of new. Journal of Medical Virology. https://doi.org/10.1002/jmv.26048
JI W, Wang W, Zhao X, Zai J, Li X. 2020a. Cross‐species transmission of the newly identified coronavirus 2019‐nCoV. Journal of Medical Virology. 92(4):433–440.
https://doi.org/10.1002/jmv.25682
JI W, Wang W, Zhao X, Zai J, Li X. 2020b. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. Journal of Medical Virology. 92(4):433-440.
https://doi.org/10.1002/fut.22099
LAU SKP, Luk HKH, Wong ACP, Li KSM, Zhu L, He Z, Fung J, Chan TTY, Fung KSC, Woo PCY. 2020. Possible bat origin of severe acute respiratory syndrome coronavirus 2. Emerging Infectious Diseases. 26(7):1542. https://doi.org/10.3201/eid2607.200092
LI Z, Yi Y, Luo X, Xiong N, Liu Y, Li S, Sun R, Wang Y, Hu B, Chen W. 2020. Development and clinical application of a rapid IgM‐IgG combined antibody test for SARS‐CoV‐2 infection diagnosis. Journal of Medical Virology. 92(9):1518–1524.
https://doi.org/10.1002/jmv.25727
LIU P, Jiang JZ, Wan XF, Hua Y, Li L, Zhou J, Wang X, Hou F, Chen J, Zou J. 2020. Are pangolins the intermediate host of the 2019 novel coronavirus (SARS-CoV-2)?. PLoS Pathogens. 16(5):e1008421. https://doi.org/10.1371/journal.ppat.1008421
LOTFI M, Rezaei N. 2020. SARS‐CoV‐2: a comprehensive review from pathogenicity of the virus to clinical consequences. Journal of Medical Virology. 92(10):1864–1874.
https://doi.org/0000-0002-3836-1827
LU S, Zhao Y, Yu W, Yang Y, Gao J, Wang J, Kuang D, Yang M, Yang J, Ma C. 2020. Comparison of SARS-CoV-2 infections among 3 species of non-human primates. BioRxiv. https://doi.org/10.1101/2020.04.08.031807
MAJUMDER J, Minko T. 2021. Recent Developments on Therapeutic and Diagnostic Approaches for COVID-19. The AAPS Journal. 23(1):1–22.
https://doi.org/10.1208/s12248-020-00532-2
MICHEL M, Bouam A, Edouard S, Fenollar F, di Pinto F, Mège J, Drancourt M, Vitte J. 2020. Evaluating ELISA, immunofluorescence, and lateral flow assay for SARS-CoV-2 serologic assays. Frontiers in Microbiology. 11:597529.
https://doi.org/10.3389/fmicb.2020.597529
MUNSTER VJ, Feldmann F, Williamson BN, van Doremalen N, Pérez-Pérez L, Schulz J, Meade-White K, Okumura A, Callison J, Brumbaugh B. 2020. Respiratory disease in rhesus macaques inoculated with SARS-CoV-2. Nature. 585(7824):268–272. https://doi.org/10.1038/s41586-020-2324-7
NELSON RW, Couto CG. 2019. Small Animal Internal Medicine-E-Book. Elsevier Health Sciences. ISBN 978-0-323-57014-5
NGUYEN, D, Skelly D, Goonawardane N. 2021. A Novel Immunofluorescence Assay for the Rapid Serological Detection of SARS-CoV-2 Infection. Viruses. 13(5):747.
https://doi.org/10.3390/v13050747
OIE, W. O. for A. H. (World Organisation for Animal Health). 2021a. Guidance on working with farmed animals of species susceptible to infection with SARS-CoV-2. https://www.oie.int/fileadmin/Home/MM/Draft_OIE_Guidance_farmed_animals_cleanMS05.11.pdf
OIE, W. O. for A. H. (World Organization for Animal Health). 2021b. SARS-CoV-2 in animals used for fur farming: GLEWS+ risk assessment, 20 January 2021. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-fur-farming-risk-assessment-2021.1
OIE-WAHIS. (World Organization for Animal Health). 2021. World Animal Health Information System. https://wahis.oie.int/#/events
ORESHKOVA N, Molenaar RJ, Vreman S, Harders F, Munnink BBO, Hakze-van der Honing RW, Gerhards N, Tolsma P, Bouwstra R, Sikkema RS. 2020. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Eurosurveillance. 25(23):2001005. https://doi.org/10.2807/1560-7917.ES.2020.25.23.2001005
ÖZÇÜRÜMEZ MK, Ambrosch A, Frey O, Haselmann V, Holdenrieder S, Kiehntopf M, Neumaier M, Walter M, Wenzel F, Wölfel R. 2020. SARS-CoV-2 antibody testing—questions to be asked. Journal of Allergy and Clinical Immunology. 146(1):35–43.
https://doi.org/10.1016/j.jaci.2020.05.020
PAPICH MG. 2015. Saunders handbook of veterinary drugs-e-book: small and large animal. Elsevier Health Sciences. ISBN 978-0-323-24485-5
PLUMB DC. 2018. Plumb’s Veterinary Drug Handbook: Desk. John Wiley & Sons. ISBN 978-1-1193-4445-2
PRUIJSSERS AJ, George AS, Schäfer A, Leist SR, Gralinksi LE, Dinnon III KH, Yount BL, Agostini ML, Stevens LJ, Chappell JD. 2020. Remdesivir inhibits SARS-CoV-2 in human lung cells and chimeric SARS-CoV expressing the SARS-CoV-2 RNA polymerase in mice. Cell Reports. 32(3):107940. https://doi.org/10.1016/j.celrep.2020.107940
RAVI N, Cortade DL, Ng E, Wang SX. 2020. Diagnostics for SARS-CoV-2 detection: A comprehensive review of the FDA-EUA COVID-19 testing landscape. Biosensors and Bioelectronics, 165:112454. https://doi.org/10.1016/j.bios.2020.112454
ROTHAN HA, Byrareddy SN. 2020. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. 102433.
https://doi.org/10.1016/j.jaut.2020.102433
RUIZ-ARRONDO I, Portillo A, Palomar AM, Santibanez S, Santibanez P, Cervera C, Oteo JA. 2020. Detection of SARS-CoV-2 in pets living with COVID-19 owners diagnosed during the COVID-19 lockdown in Spain: A case of an asymptomatic cat with SARS-CoV-2 in Europe. Transboundary and emerging diseases. 68(2):973-976.
https://doi.org/10.1101/2020.05.14.20101444
SALATA C, Calistri A, Parolin C, Palù G. 2019. Coronaviruses: a paradigm of new emerging zoonotic diseases. Pathogens and Disease. 77(9):ftaa006.
https://doi.org/10.1093/femspd/ftaa006
SCHLOTTAU K, Rissmann M, Graaf A, Schön J, Sehl J, Wylezich C, Höper D, Mettenleiter TC, Balkema-Buschmann A, Harder T. 2020. Experimental transmission studies of SARS-CoV-2 in fruit bats, ferrets, pigs and chickens. Lancet Microbe. 1(5):e218–e225. https://doi.org/10.1016/S2666-5247(20)30089-6
SHARUN K, Dhama K, Pawde AM, Gortázar C, Tiwari R, Bonilla-Aldana DK, Rodriguez-Morales AJ, de la Fuente J, Michalak I, Attia YA. 2021. SARS-CoV-2 in animals: potential for unknown reservoir hosts and public health implications. Veterinary Quarterly. 41(1):181–201. https://doi.org/10.1080/01652176.2021.1921311
SHEREEN MA, Khan S, Kazmi A, Bashir N, Siddique R. 2020. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research. 24(3):91-98. https://doi.org/10.1016/j.jare.2020.03.005
SHI J, Wen Z, Zhong G, Yang H, Wang C, Huang B, Liu R, He X, Shuai L, Sun Z. 2020. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science. 368(6494):1016–1020. https://doi.org/10.1126/science.abb7015
SIDIQ Z, Hanif M, KumarDwivedi K, Chopra KK. 2020. Benefits and limitations of serological assays in COVID-19 infection. Indian Journal of Tuberculosis. 67(4):S163-S166. https://doi.org/10.1016/j.ijtb.2020.07.034
SINGHAL T. 2020. A review of coronavirus disease-2019 (COVID-19). The Indian Journal of Pediatrics. 1–6. https://doi.org/10.1007/s12098-020-03263-6
SIT THC, Brackman CJ, Ip SM, Tam KWS, Law PYT, To EMW, Yu VYT, Sims LD, Tsang DNC, Chu DKW. 2020. Infection of dogs with SARS-CoV-2. Nature. 586(7831):776-778. https://doi.org/10.1038/s41586-020-2334-5
SUAREZ DL, Pantin-Jackwood MJ, Swayne DE, Lee SA, Deblois SM, Spackman E. 2020. Lack of susceptibility of poultry to SARS-CoV-2 and MERS-CoV. BioRxiv. https://doi.org/10.1101/2020.06.16.154658
SUN J, He WT, Wang L, Lai A, Ji X, Zhai X, Li G, Suchard MA, Tian J, Zhou J. 2020. COVID-19: epidemiology, evolution, and cross-disciplinary perspectives. Trends in Molecular Medicine. 26(5):483–495. https://doi.org/10.1016/j.molmed.2020.02.008
TANG X, Wu C, Li X, Song Y, Yao X, Wu X, Duan Y, Zhang H, Wang Y, Qian Z. 2020. On the origin and continuing evolution of SARS-CoV-2. National Science Review. 7(6):1012–1023. https://doi.org/10.1093/nsr/nwaa036
TIWARI R, Dhama K, Sharun K, Iqbal Yatoo M, Malik YS, Singh R, Michalak I, Sah R, Bonilla-Aldana DK, Rodriguez-Morales AJ. 2020. COVID-19: animals, veterinary and zoonotic links. Veterinary Quarterly. 40(1):169-182.
https://doi.org/10.1080/01652176.2020.1766725
WHO. (World Health Organization). (2020). COVID 19 Public Health Emergency of International Concern (PHEIC). Global research and innovation forum: towards a research roadmap. https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum
WHO. (World Health Organization). 2021. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/
WONG G, Bi YH, Wang QH, Chen XW, Zhang ZG, Yao YG. 2020. Zoonotic origins of human coronavirus 2019 (HCoV-19/SARS-CoV-2): why is this work important?. Zoological Research. 41(3): 213. https://doi.org/10.24272/j.issn.2095-8137.2020.031
WOODBY B, Arnold MM, Valacchi G. 2020. SARS‐CoV‐2 infection, COVID‐19 pathogenesis, and exposure to air pollution: What is the connection?. Annals of the New York Academy of Sciences. 1486(1):15-38. https://doi.org/10.1111/nyas.14512
WROBEL AG, Benton DJ, Xu P, Roustan C, Martin SR, Rosenthal PB, Skehel JJ, Gamblin SJ. 2020. SARS-CoV-2 and bat RaTG13 spike glycoprotein structures inform on virus evolution and furin-cleavage effects. Nature Structural & Molecular Biology. 27(8):763–767. https://doi.org/10.1038/s41594-020-0468-7
XIAO K, Zhai J, Feng Y, Zhou N, Zhang X, Zou JJ, Li N, Guo Y, Li X, Shen X. 2020. Isolation of SARS-CoV-2-related coronavirus from Malayan pangolins. Nature. 583(7815):286-289. https://doi.org/10.1038/s41586-020-2313-x
XIE E, Guangzhou GRI. 2020. Why wild animals are a key ingredient in China’s coronavirus outbreak. Australasian Policing. 12(2):8.
https://search.informit.org/doi/10.3316/informit.217111399726998
YE ZW, Yuan S, Yuen KS, Fung SY, Chan CP, Jin DY. 2020. Zoonotic origins of human coronaviruses. International Journal of Biological Sciences. 16(10):1686.
https://doi.org/10.7150/ijbs.45472
ZHANG T, Wu Q, Zhang Z. 2020. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Current Biology. 30(7):1346-1351.e2.
https://doi.org/10.1016/j.cub.2020.03.022
ZHAO Y, Wang J, Kuang D, Xu J, Yang M, Ma C, Zhao S, Li J, Long H, Ding K. 2020. Susceptibility of tree shrew to SARS-CoV-2 infection. Scientific Reports. 10(1):1–9. https://doi.org/10.1038/s41598-020-72563-ww
ZHENG J. 2020. SARS-CoV-2: an emerging coronavirus that causes a global threat. International Journal of Biological Sciences. 16(10):1678-1685.
https://doi.org/10.7150/ijbs.45053
ZOETIS. 2021. Zoetis’ Emerging Infectious Disease Capabilities Support COVID-19 Solutions for Great Apes and Minks [Commercial]. https://www.zoetis.com/news-and-media/feature-stories/posts/zoetis-emerging-infectious-disease-capabilities-support-covid-19-solutions-for-great-apes-and-minks.aspx